MRCO BLOG
Medical Musings, Health Hypotheses & Therapeutic Thoughts
|
Dr. Edmund Bruce-Gardner
9/10/2018 What is Chronic Pain?NOTE: This blog post is essentially a copypasta of the page on the same topic; but it is so important a subject I wanted to make the information was available to all of our blog subscribers as well... Chronic PainWhen we talk about 'chronic pain', we're not just talking about pain that has been going on for a long time; although that it is part of the definition. Chronic pain, in this sense, involves changes to the way that information is carried and processed in our bodies. To understand this a little better, we will have to consider (briefly!) the nature of pain and what it means. Pain is an output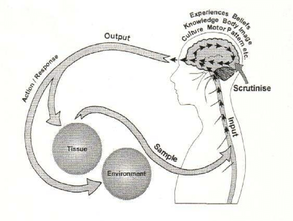 From Gifford (1998) From Gifford (1998) What this means is that all pain is produced by your central nervous system; that is, pain is the label your brain applies to information it really wants you to pay attention to. When you injure yourself, like burning your hand on a hotplate, your nerves send signals up to your spinal cord and brain. We call this nociception, or something like 'detection of something harmful or noxious'. Your brain then decides whether or not to call those signals 'pain'. From this point of view, the pain itself is just as real in something like phantom limb pain (when you (e.g.) have an arm amputated but can still feel pain in the hand) as when you accidentally stab yourself in the thigh while cutting a recipe out of a magazine (just a random example that sprang to mind). So pain is not something you feel in your body, it is something that is created and projected out by your brain. Put simply, it is an output, not an input. Pain is an evolutionary strategy In the case of touching your hand to a hot stove, you have already started moving your hand away by the time you feel the pain. What the pain is intended to do is to point out to you that your unprotected hand is not the best way to turn that pancake, and that maybe next time you should use a spatula! So the memory of pain makes us less likely to try and use our digits as kitchen utensils in the future as well as making us stop the behaviour causing the pain in the first place. It also makes you take care of an area while it is healing, so serves a protective function. So pain is just a warning signal, and in normal circumstances, it is a good thing. Another way of saying this is that it is a adaptive strategy, or one that makes you more likely to stay alive. People who can't feel pain for one reason or another run a very real risk of ignoring a seemingly small injury that then becomes infected, and possibly life-threatening. Pain is normal! Image by Studio224 Image by Studio224 Leading on from the above two points, it should be clear that pain is a normal function of our bodies when everything is working as it should, albeit one most of us don't really want! It is meant to be unpleasant, otherwise it wouldn't work the way it does. Pain is what we experience when our brains have decided we are threatened or in danger, and wants us to do something about it. In the case of chronic pain, where the pain has persisted long past the point where we might have expected any injury to heal, the key is to identify why the brain feels threatened. 'Pain' is, tellingly, also used with respect to grief or loss, or loneliness. This emotionally-laden 'pain' is crucial in understanding chronic pain - indeed, all pain! - as it reinforces the idea that these sensations are the result of many different inputs, and our emotions, thoughts, beliefs and behaviours are all important contributors to how we experience pain. Pain and damage are not necessarily related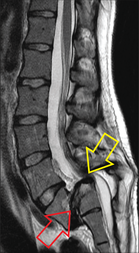 This image is from an asymptomatic 32 year old female. The red arrow shows where the spine has slipped forwards, the yellow points to the spinal cord doing a slalom around the step like an Olympic skiier! From Eliott et al (2010) This image is from an asymptomatic 32 year old female. The red arrow shows where the spine has slipped forwards, the yellow points to the spinal cord doing a slalom around the step like an Olympic skiier! From Eliott et al (2010) This starts to explain the idea that pain is an output, where trauma or tissue damage is not the only factor (as mentioned over on the page on age-related conditions like arthritis.) We know from decades of medical imaging that people can have the most spectacular structural failures, like compression of the spinal cord or broken bones, and experience little to no pain or dysfunction. Sheehan (2010) for example, found that among asymptomatic (i.e. not having any symptoms) 60 year-olds, over 90% had degenerative or bulging discs. 21% had spinal stenosis, narrowing of the hollow middle bit of the spinal column, where your spinal cord sits. One might imagine that squishing your spinal cord would result in some sort of symptoms, but not necessarily! See the image on the left for a truly mindboggling scan of a compressed spinal cord that did not result in any pain at all (they had the scan done for other reasons). Anecdotal reports from wounded in wartime often describe bullet wounds and even severe trauma as an impact, like being bumped or knocked in a crowd. At the other end of the spectrum, consider a paper cut. If pain is just an evolutionary mechanism to warn you about damage, why does the bloody thing hurt so much! It is not deep, or (under normal circumstances) anything close to a serious danger to the body, but we react as if it was the next thing to losing a limb. Chronic Pain
 So how can osteopathy help? An analogy I often use with my patients is to think about your central nervous system (or CNS, consisting of your brain and spinal cord) as a genius four year-old. It is incredibly discriminating and intelligent in some ways, and unsophisticated and stupid in others. Like a four year-old, it also has a tendency to throw tantrums (overreact with pain, for example). And also like a four year-old, the best way of getting through to it is repetition. By repeatedly moving and stretching areas where the body perceives pain, we can increase the 'positive feedback' coming from that area. "Look, we are moving this painful shoulder in all these different ways, and the arm has not fallen off! Maybe it's OK to decrease the number of pain labels we are attaching to this area. Maybe it's OK to relax a little!" This makes the CNS feel a little safer. We can also help you with some of the other facets of your pain. The folks over at NOI (the neuro-orthopaedic institute) have come up with this wonderful concept of DIMs ("Dangers In Me") and SIMs (Safeties in me) that can help identify unhelpful and helpful factors in your life that influence whether or not you feel pain. The more factors we can identify, the more chance we have of helping you get your CNS to a place where it feels safe, and where you do not feel pain. References Eliott, JM, Fleming, H & K Tucker (2010) "Asymptomatic spondylolisthesis and pregnancy" J Ortho Sports Phys Ther 40:324 Gifford, LS (1998) "Pain, the tissues, and the nervous system: a conceptual model" Physiotherapy 84(1):27-36 Sheehan, NJ (2010) "Magnetic resonance imaging for low back pain: indications and limitations" Ann Rheum Dis 2010; 69:7-11 Special mentions to The Sensitive Nervous System (Butler et al, 2000) and Explain Pain Supercharged (Butler et al, 2017), which are great resources around explaining both central and peripheral nueropathic pain and have informed my whole approach to chronic pain management. Dr. Edmund Bruce-Gardner The knee is a pretty badly-designed joint. Evolution doesn't move towards perfection, but function. As bipedal (two-legged) creatures who evolved from quadrupedal (four-legged) ones, quite a few compromises and fudges have been made. [The shoulder is another good example. it is a heavily-modified hip (i.e. ball-and-socket joint), but one where the bony shape and supporting ligaments have to allow for such a large range of motion that it relies on the surrounding muscles for nearly all of its support and integrity, as well as on the function of all the other joints surrounding it. You can read more about the weird and wonderful world of the shoulder complex here.] But anyway, the knee... It is a hinge joint, the largest joint in the body, sandwiched in between the two longest bones in the human body, the femur (thigh bone) and tibia (shin bone). This is a fairly bad idea to start with, because long levers generate a lot of force. Worse, it's not a very simple hinge joint. If it were, and could only bend forwards and backwards, and we wouldn't be able to walk on broken or uneven ground. So we have the longest bones (/levers), generating a huge amount of force, going into the largest joint, which is also extremely complex.  Doesn't look massively stable, does it? Doesn't look massively stable, does it? Back when we put all of our weight through four ‘knees’ instead of two, this was less of an issue. We also tend to weight-bear with our knees more or less unbent. This provides a lot more opportunity for trauma. Contrast this with other mammals such cats, dogs, horses, chipmunks, etc. etc. The bottom of the thigh bone is a bit like the cartoon version of a bone, with two knobbly bits (called condyles) at the bottom. These then (theoretically) meet, or articulate, with the relatively flat top of the shin bone. This works about as well as you would imagine. 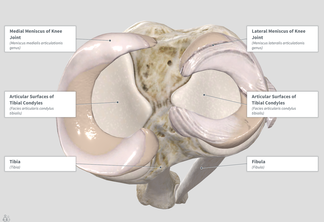 Evolution’s workaround here was to put these two sort of cups, called menisci, on the top of the flat bit of the shin bone (rather poetically called the tibial plateau). These allow the knobbly condyles to sit a bit more firmly on the top of the tibia. Now, of course, we have another structure that takes a lot of force, and can get injured. Most sports fans (not to mention players) will have heard of a torn meniscus. I tore mine when I was about fourteen, and still remember it as one of the most exquisitely painful experiences of my life. As you can see in the diagram above, when the menisci (the 'C-shaped' things around the outside) are in place they cover most of the top of the tibial plateau.  Here you can see the collateral ligaments (on the sides) and sneak a peek of the cruciate ligaments and menisci (between the femur and tibia) Here you can see the collateral ligaments (on the sides) and sneak a peek of the cruciate ligaments and menisci (between the femur and tibia) But wait! There's more! It's not all about the menisci. In a flash of evolutionary genius, the other main way that the knee is stabilised is by four... ...elastic bands, Well, not literally, but they might as well be. The rubber bands (known as ligaments by the medical types) are actually just thickenings of the capsule that surrounds the joint. Again, sports buffs will probably recognise the terms medial and lateral collateral ligaments. These refer to the ligaments on the inside, and outside, of the knee, respectively. The anterior and posterior cruciate (or 'cross-like') ligaments go between the femur and tibia, and can be seen (along with the menisci) sandwiched in there on the left. So we have this large, unstable joint subject to huge forces, that we hold in biomechanically-compromised positions. Hmmmm, what could go wrong?
All joking aside, we will go into some of the ways the knee (and associated structures) can start breaking bad. Stay tuned for my series on the knee, which will hopefully be completed at a slightly less glacial pace than the shoulder! |
AuthorsDrs. Edmund Bruce-Gardner and Soraya Burrows are osteopaths Categories
All
|
|
Osteopathy at Moreland Road Clinic
High quality & personalised service from experienced professionals. A safe, effective & collaborative approach to patient care. All osteopaths undertake a 4-5 year university degree and are licensed and registered healthcare pracitioners. |
Find Us
Moreland Road Clinic 85 Moreland Road Coburg VIC 3058 P (03) 9384 0812 F (03) 9086 4194 osteopathy@morelandroadclinic.com.au |
Popular Blog Posts
|
|
|
Osteopathy at Moreland Road Clinic is on Moreland Road, near the corner of Nicholson Street/Holmes Street, on the border of Coburg, Brunswick & Thornbury.
This makes Osteopathy at Moreland Road Clinic the ideal location for people in the inner north and outer northern suburbs of Melbourne, including: Coburg, Coburg North, Coburg East, Brunswick, Brunswick East, Brunswick West, Fawkner, Oak Park, Glenroy, Preston, Pascoe Vale, Pascoe Vale South, Gowanbrae, Hadfield, Essendon, Moonee Ponds, Thornbury and Reservoir. |
12/2/2019
0 Comments